70YR OLD MALE WITH FACIAL PUFFINESS,ABDOMINAL DISTENSION
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
Name : Supriya .K ( Intern )
Roll Number : 63
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
70YR OlD MALE from Valigonda ,who is daily wage labourer by Occupation, came with C/O Facial puffiness , Distension of abdomen , Swelling of Left LL and Right UL Since 1 month .
BIOLOGICAL COMPONENT :
Patient was apparently asymptomatic 20years ago , then he developed difficultly /Pain during walking (used painkillers) ,following which patient developed deformity of B/L Knee and was suggested Surgery .(then ,he used to walk with Support ,Now he is Crawling )
H/O trauma + during Childhood .
5 Years ago - he developed Facial Puffiness ,Distension of abdomen ,swelling of limbs , Fever ,SOB , Decreased urine output and decreased bowel movements and diagnosed to have Pneumonia and was started on conservative management and resolved .
3 Years ago - H/O similar complaints and got admitted for 1 week and got treated conservatively
Blackish Discoloration of skin ( Change in the skin tone ) developed since 6 months .
1 month ago - He developed fever ,which was sudden in onset , intermittent type ,low grade , associated with chills , relieved on taking medication ,also developed SOB - Grade II (MMRC) ,Orthopnoea + , PND -
Generalised swelling (ANASARCA ) since 1 month , Subsided after 2-3 weeks with medication .
Hoarseness of Voice developed Since 1 month .
Mixed Diet ( Allergic to Chicken -as they observed edematous changes after having it since 6months) , Occasional alcoholic , Chews Betel leaf + Tobacco (Pan) Since Childhood (15yrs )
PSYCHO-SOCIAL COMPONENT :
Inputs,Obtained from his Wife - Most active (60YR OLD, who is daily wage worker by Occupation, Not Educated but speaks Hindi ,Telugu , Understands some words in English and Speaks some words also - She said Thank You(English ) to me after Conversation) ,and Cheerful women who always keep smiling ,Loved speaking with her (felt happy)
70YR Old Male Patient ,who is a daily wage labourer by Occupation,who worked in the Construction Sites Under Builder at Mumbai .
He stayed at Mumbai, along with his family Since very young age , Built their Own small House at Mumbai in 1980s but not registered.
He has 4 Children :
1st Child - Daughter 40YR Old now has 2 Children ,Stays in Hyderabad
2nd Child - Son 38YR Old now , has 2 children ,Stays at Valigonda
3rd Child - Daughter - EXPIRED 14 Years ago , due to Liver failure .( Spent nearly 1 Lakh to save her - though belonging to below Middle Class ) - She had 2 children (daughter and son ) Her Husband married to another lady - She also Expired (Suicide) - had 1 son
4th Child - Son - 32YR OLD - has 2 children - 2 Sons ,Stays at Mumbai .
He got retired 20years ago , Came to his Native place ,Valigonda and started living with his Elder Son family(consanguenous marriage ) as his Daughter in Law belongs to their family ,She always took care of him like a daughter since 20years .As His wife used to stay at Mumbai with their younger son ,till his marriage and then came back to her husband 10years ago .
Maintains Personal Hygeine and Cleanliness to extreme end -His clothes should be very neat ,shaves his beard every 2 times in a week ,takes bath regularly for 30-40mints , sometimes he washes his own clothes despite of his knee deformity .
His First complaint ,B/L knee pain started in the last year before retirement .Since then he used pain killers ,firstly his U/L knee affected, gradually lead to B/L knee pain and deformity ----> lead to Walk with Support (Stick) ------> Walk with Support (Stand ) --------> Crawling .
whatever may be his health condition and his posture and gait --- He is a happy going ,Cheerful person , who always speaks with love to everyone ,even with strangers ,Despite of Conductive hearing loss since 10years .
No Personal and Professional stressors present ( according to his Wife ).
PAST HISTORY:
K/C/O Hypertension Since 3 Years ( Under TAB TELMA 20MG PO/OD )
N/K/C/O DM-2 ,Asthma ,TB , Epilepsy .
PERSONAL HISTORY :
Appetite -Normal
Diet - Mixed
Sleep - adequate
Bladder movements - Nocturia , Hesitancy , Urgency + since 2 months .
Bowel movements - regular
Addictions - Occasional Alcoholic,chews tobacco+ betel nut (since age -15 years )
GENERAL EXAMINATION:
Patient is conscious,coherent , irritable
Pallor - Absent
Icterus - Absent
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy - Absent
Edema - Facial puffiness ,abdominal distension and limbs swelling
Temp : Afebrile
BP : 110/70mmHg
PR : 76bpm
RR : 22cpm
SpO2 : 96% On RA
I/O : 950 /900 ml
GRBS : 95mg/dl
Systemic Examination:
CVS : S1 S2 + ,No murmurs .
RS : BAE + , Tenderness + over B/L 4th ,5th ICS
CNS : HMF intact , NAD
P/A : Soft ,Distended ,Non tender
SYSTEMIC EXAMINATION:
ON INSPECTION:
Abdomen - mildly distended
umbilicus is inverted
Skin over abdomen is normal
No visible pulsations
No engorged veins
PALPATION :
all inspectory findings confirmed
No rise of temperature and tenderness
No guarding and rigidity
No hepatomegaly and Splenomegaly
PERCUSSION :
Shifting dullness - absent
Fluid thrills - absent
Puddle sign cannot be elicited ,as pt is not co-operative
AUSCULTATION:
Bowel sounds - heard
No Bruits
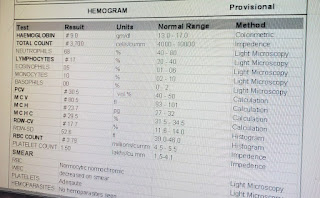
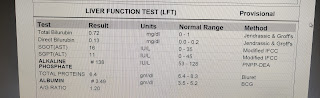
INVESTIGATIONS:
2D ECHO :
USG ABDOMEN:
SOAP NOTES:
AMC
DAY -3
BED- 1
UNIT - 3
S
No fever spikes
Stools passed
O
Patient is conscious,coherent , irritable
Temp : Afebrile
BP : 120/70mmHg
PR : 96bpm
RR : 22cpm
SpO2 : 95% On RA
CVS : S1 S2 + ,No murmurs ,JVP raised
RS : BAE + , Tenderness + over B/L 4th ,5th ICS
CNS : HMF intact , NAD
P/A : Soft ,Distended ,Non tender
A
ANASARCA UNDER EVALUATION,SECONDARY TO HEART FAILURE WITH MID RANGE EJECTION FRACTION (45%) WITH NON OLIGURIC AKI ON ? CKD WITH SOLITARY THYOID NODULE OF LT LOBE WITH GRADE II PROSTATOMEGALY
K/C/O HTN SINCE 3YEARS
P
Fluid Restriction <1.5 Lit/day
Salt Restriction < 2 gms /day
Inj .Lasix 40mg IV /BD
Tab. Carvidas 3.125 mg PO/BD
Tab. Telma H 20mg PO/OD
Tab. Ecospirin AV 75/10 PO/HS
Tab. Aldactone 50mg PO/OD
Tab. Ultracet 1/2 Tab PO/QID
Strict I/O Charting
Vitals Monitoring 4th hrly
AMC
DAY -4
BED- 1
UNIT - 3
S
No fever spikes
Stools passed
O
Patient is conscious,coherent , irritable
Temp : Afebrile
BP : 110/70mmHg
PR : 76bpm
RR : 22cpm
SpO2 : 96% On RA
I/O : 950 /900 ml
GRBS : 95mg/dl
CVS : S1 S2 + ,No murmurs .
RS : BAE + , Tenderness + over B/L 4th ,5th ICS
CNS : HMF intact , NAD
P/A : Soft ,Distended ,Non tender
A
ANASARCA ,SECONDARY TO HEART FAILURE WITH MID RANGE EJECTION FRACTION (45%) WITH NON OLIGURIC AKI ON ? CKD ,ANEMIA UNDER EVALUATION ? SECONDARY TO ANEMIA OF CHRONIC DISEASE WITH SOLITARY THYOID NODULE OF LT LOBE WITH GRADE II PROSTATOMEGALY
K/C/O HTN SINCE 3YEARS
P
Fluid Restriction <1.5 Lit/day
Salt Restriction < 2 gms /day
Inj .Lasix 40mg IV /BD
Tab. Carvidas 3.125 mg PO/BD
Tab. Telma H 20mg PO/OD
Tab. Ecospirin AV 75/10 PO/HS
Tab. Aldactone 50mg PO/OD
Tab .Tamsulosin 0.4mg PO/OD
Tab. Ultracet 1/2 Tab PO/QID
Tab . Gabapentin 300mg PO/OD
Strict I/O Charting
Vitals Monitoring 4th hrly
WARD
DAY -5
UNIT - 3
S
No fever spikes
Stools not passed ,Flatus passed
O
Patient is conscious,coherent , cooperative
Temp : Afebrile
BP : 120/70mmHg
PR : 78bpm
RR : 22cpm
GRBS : 95mg/dl
CVS : S1 S2 + ,No murmurs .
RS : BAE + , Tenderness decreased over B/L 4th ,5th ICS
CNS : HMF intact , NAD
P/A : Soft ,Non tender
A
ANASARCA ,SECONDARY TO HEART FAILURE WITH MID RANGE EJECTION FRACTION (45%) SECONDARY TO CAD WITH NON OLIGURIC AKI ON ? CKD WITH ANEMIA UNDER EVALUATION ? SECONDARY TO ANEMIA OF CHRONIC DISEASE WITH SOLITARY THYOID NODULE OF LT LOBE WITH GRADE II PROSTATOMEGALY
WITH DENOVO HYPOTHYROIDISM
K/C/O HTN SINCE 3YEARS
P
Fluid Restriction <1.5 Lit/day
Salt Restriction < 2 gms /day
Inj .Lasix 40mg IV /BD
Tab. Carvidas 3.125 mg PO/BD
Tab. Telma H 20mg PO/OD
Tab. Ecospirin AV 75/10 PO/HS
Tab. Aldactone 50mg PO/OD
Tab .Tamsulosin 0.4mg PO/OD
Tab . Thyronorm 25mcg PO/OD
Tab. Ultracet 1/2 Tab PO/QID
Tab . Gabapentin 300mg PO/OD
Strict I/O Charting
Vitals Monitoring 4th hrly
WARD
DAY -6
UNIT - 3
S
No fever spikes
Stools not passed ,Flatus passed
O
Patient is conscious,coherent , cooperative
Temp : Afebrile
BP : 120/70mmHg
PR : 84bpm
RR : 20cpm
CVS : S1 S2 + ,No murmurs .
RS : BAE + , Tenderness decreased over B/L 4th ,5th ICS
CNS : HMF intact , NAD
P/A : Soft ,Non tender
A
ANASARCA ,SECONDARY TO HEART FAILURE WITH MID RANGE EJECTION FRACTION (45%) SECONDARY TO CAD WITH NON OLIGURIC AKI ON ? CKD WITH ANEMIA UNDER EVALUATION ? SECONDARY TO ANEMIA OF CHRONIC DISEASE WITH SOLITARY THYOID NODULE OF LT LOBE WITH GRADE II PROSTATOMEGALY
WITH DENOVO HYPOTHYROIDISM
K/C/O HTN SINCE 3YEARS
P
Fluid Restriction <1.5 Lit/day
Salt Restriction < 2 gms /day
Inj .Lasix 40mg IV /BD
Tab. Carvidas 3.125 mg PO/BD
Tab. Telma H 20mg PO/OD
Tab. Ecospirin AV 75/10 PO/HS
Tab. Aldactone 50mg PO/OD
Tab .Tamsulosin 0.4mg PO/OD
Tab . Thyronorm 25mcg PO/OD
Tab. Ultracet 1/2 Tab PO/QID
Tab . Gabapentin 300mg PO/OD
Strict I/O Charting
Vitals Monitoring 4th hrly





























Comments
Post a Comment