Online blended bimonthly assignment toward summative assessment for the month of May 2021
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link of the questions asked regarding the cases
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
) Pulmonology (10 Marks)
A) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer : Evolution of symptomatology:
Shortness of breathe - 1st episode(primary exposure to the allergen)- 20 years back- made her sensitized to the allergen
Every year she had the same situation at the time of paddy field dust exposure
Subsequent exposures of sensitized allergens resulted in bronchoconstriction and airway passage narrowing - which resulted in shortness of breathe and dyspnoea
For which she took medicines and got relief
Triggered by winter season and paddy field dust exposure/inhalation
Latest episode- 30 days back
Her HRCT showed signs of bronchiectasis which might be due to exposure to the allergen (paddy dust) every year at the same season.
Pedal edema from 15 days pitting type till ankle length
Facial puffiness from 15 days
Anatomical localization of shortness of breathe might be the lower respiratory tract system as per my knowledge.
Primary etiology- seasonal exposure to paddy field dust exposure/inhalation(TYPE I HYPERSENSITIVITY)
During an anaphylactic reaction the patient may experience hypotension, difficulty in breathing or hypoxia, and/or circulatory failure(distributive shock)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer : Placebo has no pharmacological and non pharmacological interventions, it is given for the sake of patient's well being to maoe patient stable mentally.
The various pharmacological and non pharmacological interventions used in this patient over placebo have more efficacy as they helps in decreasing the pathology, improving symptoms, and helps in recovery are as follows:
Pharmacological interventions:
1. O2 Inhalation and intermittent BIPAP
Helps with oxygenation in hypoxic and dyspnic patients. To increase SpO2 BIPAP maintains consistent breath pattern.
Indicated because there is shortness of breathe and dyspnoea
2. AUGMENTIN and AZITHROMYCIN
kills pathogenic organisms which caused the disease.
Indicated as antibiotic for both treatment and prophylaxis.
3. LASIX
loop diuretic, inhibits Na+/K+/2Cl- pump
Indicated to resolve edema and hypotension
4. PANTOP
Proton pump inhibitor, decreases secretion of HCl
Indicated as prophylaxis given along with other medications to prevent ulcers
5. HYDROCORTISONE
steroid, reduces inflammation through multiple signal transduction pathways
Indicated to reduce the anaphylactic reactions
6. Nebulization with IPRAVENT and BUDECORT
delivers the liquid droplets creating aerosols which are easy to breathe into the lungs
Indicated as patient is with severe dyspnoea
7. PULMOCLEAR
Clears the mucus in bronchi and bronchioles
Indicated to clear the air passage and help in making respiratory tract functional
8. HAI
substitutes insulin in the body
Indicated for diabetes control and along with steroids as steroid administration causes hyperglycemia
9. THIAMINE
To prevent thiamine deficiency which may result in neurological disorders
Non pharmacological interventions:
1.Head end elevation:
Significantly increases end expiratory lung volume and improves lung volumes, reduces aspiration and improves oxygenation and hemodynamic performance
Indicated for patients on ventilation and severe dyspnoea pneumonia
2. Vitals monitoring
Indicated in patients who are comorbid like hypertension, diabetes, fever, cardiovascular diseases, and who's condition is severe
3. I/O Charting
Indicated in patients who are hypertensive, diabetic or with any other renal problems.
4. Chest physiotherapy
Improves lung function and helps to breathe better
Indicated to improve lung functioning
5. GRBS 6 hourly
Indicated for patients who are prediabetic and diabetic and also who are on steroid therapy
3) What could be the causes for her current acute exacerbation?
Answer: Exposure to the allergen with her immunocompromised state (diabetis and hypertensive) she might have taken steroids for past 20 years for relief from shortness of breathe, which might have resulted in the immunocompromised state which might have caused acute exacerbation
The risk for annual recurrence for anaphylaxis was found to be about 18% in over 300 patients identified in a prospective study
Link: O'Keefe A, Clarke A, St Pierre Y, Mill J, Asai Y, Eisman H, La Vieille S, Alizadehfar R, Joseph L, Morris J, Gravel J, Ben-Shoshan M. The Risk of Recurrent Anaphylaxis. J Pediatr. 2017 Jan;180:217-221. [PubMed]
4. Could the ATT have affected her symptoms? If so how?
Answer: Yes ATT affected her symptoms
*Isoniazid and rifampcin -nephrotoxic - raised RFT was seen
5.What could be the causes for her electrolyte imbalance?
Answer: Hyponatremia:
> Worsening of Hypoxia
> Respiratory acidosis
> Right heart failure
2) Neurology (10 Marks)
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer : Evolution of symptomology;
1 year ago-2 to 3 episodes of seizures
4 months ago-Following cessation of alcohol he developed seizures probably GTCS
9 days back-The patient started talking and laughing to himself
withdrawal seizures are triggered by neuronal networks in the brainstem, including the inferior colliculus.
Ethanol is the primary alcohol ingested by chronic users. It is a central nervous system (CNS) depressant that the body becomes reliant on with extended exposure to ethanol. It does this by inhibiting the excitatory portion (glutamate receptors) of the CNS and enhancing the inhibitory portions (GABA receptors) of the CNS. When the depressant is stopped, the central nervous system becomes overexcited as the inhibition is taken away. Thus, the body gets an excitatory overload, which results in the symptoms of withdrawal
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer : As the aim of lowering the alcohol levels and its metabolites ,its neuro deppresive effects
and making patients spnding less in the ED
THIAMINE -
mechanism of action ;combines with adenisine tri phosphate in the liver. and it has no effect onthe symptoms and signs of the alcohol withdrawl .or on the incidence of the seizuers . routine use of the thiamine is recomended because the development of Wernicke encephalopathy or Wernicke-Korsakoff syndrome is disastrous in these patients and can remain unrecognized. Because orally administered thiamine may have poor enteral absorption in individuals with alcoholism, high-risk patients should receive parenteral thiamine at 100-250 mg once daily for several days.
LORAZEPAM; it was by the rehab facilities across the nations to help patients overcome the AUD
As the mechanism of action it binds to the benzodizepam receptors on the post synaptic GABA ligand gated channels.
the indications are active seizures ,severe anxiety.
Efficacy; it is used to treat all the seizuers
PREGABALIN; It was the high α2δ voltage gated channel subunit ligand and acounting for there actions invivo to reduce neuronal excitability and seizures
Potchlor Potklor liquid is used to treat low levels of potassium in the body
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Answer : due to the excess thalamine deficiency and excess toxins accumalation and due to renal disease caused by excess alcohol addiction
4) What is the reason for giving thiamine in this patient?
Answer : chronic alcohol cosumption causes thalamine deficiency due to impaired absorbstion of thalamine from the intestine A number of mechanisms may be involved in the pathogenesis of thiamin deficiency in the alcoholic population. An important cause is inadequate intake of thiamin. Moreover, there may be decreased conversation of thiamine to the active coenzyme, reduced hepatic storage of the vitamin in patients with fatty metamorphosis, ethanol inhibition of intestinal thiamine transport, and impaired thiamine absorption secondary to other states of nutritional deficiency
5) What is the probable reason for kidney injury in this patient?
Answer : Mechanical ventilation was an important treatment for patients with AECOPD.13 On the contrary, mechanical ventilation was also an independent risk factor for AKI.
6). What is the probable cause for the normocytic anemia?
Answer : Anemia of chronic disease (ACD) is probably the most common type of anemia associated with COPD. ACD is driven by COPD-mediated systemic inflammation. Anemia in COPD is associated with greater healthcare resource utilization, impaired quality of life, decreased survival, and a greater likelihood of hospitalization. Anemia was normocytic and normochromic in nature. The exact cause of anemia of chronic disease may vary. Anemia can be caused by a slight shortening of normal red blood cell survival. the production of red blood cells (erythropoiesis) or erythropoietin (a hormone that stimulates red blood cell production) may be impaired.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Answer : Oxygen is important for cell metabolism and is critical for all wound-healing processes Inhibits wound healing by reducing the quantity and quality of oxygen to the wound site.
B) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :7 days back- Giddiness and 1 episode of vomiting
Asymptotic for 3 days
4 days back-Giddiness (sudden continuous and gradually progressive)
Bilateral hearing loss with aural fullness and tinnitus
Vomitings 2-3 episodes per day(non projectile non bilious with food particles
Postural instability Unable to walk without support and is swaying with tendency to fall while walking
Anatomical localisation
Cerebellum which is responsible for postural stability ,ocular movements and vertigo(central)
usually results from damage to the part of your brain that controls muscle coordination (cerebellum). conditions can cause ataxia, including alcohol misuse, certain medication, stroke, tumor, cerebral palsy, brain degeneration and multiple sclerosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer :Vertin Tablet is employed to stop and treat a disorder of the internal ear referred to as disease. The symptoms include dizziness (vertigo), ringing within the ears (tinnitus), and loss of hearing, probably caused by fluid within the ear. This medicine helps relieve the symptoms by reducing the number of fluid.
Zofer anti-emetics' primarily utilized in the prevention of vomiting (being sick) and nausea (feeling sick) that typically occur after cancer chemotherapy, radiation treatment or surgery.
Ecosporin commonly used for the diagnosis or treatment of Headache, migraine, fever, pharyngitis, neuralgia
Atorvostatin
Statins are effective in reducing both first-ever and recurrent stroke, and this effect seems driven by the extent of LDL-C lowering
Clopidogrel could be a variety of medicine called an antiplatelet: it reduces the danger of blood clots forming within your vascular system or blood vessels.
Mvt Methylcobalamin is employed in cyanocobalamin deficiency.
Methylcobalamin could be a kind of vitamin B that restores its level within the body thereby helping in treating certain anemias and nerve problems
3) Did the patients history of denovo HTN contribute to his current condition?
Answer : Raised blood pressure (BP) is common after stroke but its causes, effects, and management still remain uncertain.It exists in more than three quarters of patients, of which about half have a history of hypertension [1], and it declines spontaneously in two-thirds of cases returning to prestroke levels over the first week. Its decrease usually occurs 4–10 days after stroke, but in a significant percentage of patients it falls by about 25–30% just within the first 24 hours; particularly when they are moved to a quiet room, they are allowed to rest and their bladder is empty.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Answer : Yes, Atrial fibrillation and alcohol Drinking excessive amounts of alcohol can trigger atrial fibrillation – a type of irregulaR heartbeat. Atrial fibrillation increases your risk of stroke by five times, because it can cause blood clots to form in the heart. If these clots move up into the brain, it can lead to stroke.
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :Evolution of symptomatology
Bilateral pedal edema from 8 months (releiving by medications and recurring)
There is dyselectrolytemia too
Edema is recurring frequently and subsides on medication. But there is no potassium supplementation
This hypokalemia led to improper cardiac functioning which led to palpitations .and also leads to difficulty in breathing
Because of this palpitations, which might have resulted in chest pain and pain in the left upper limb
This hypokalemia might have resulted in paresis of limbs
Symptoms of hypokalemia may include attacks of severe muscke weakness, eventually leading to paralysis and possibly respiratory failure.
Anatomical localization: electrolyte imbalance in body affecting cardiovascular system
Primary etiology: hypokalemia
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Answer : Might be due to the usage of steroids from 8 months for relief from edema.
Recently it has been reported that the beneficial effect of steroids might be attributed to inhibition of edema spread or acceleration of edema resorption
Oral or IV steroids with glucocorticoid properties, such as prednisone and hydrocortisone sometimes used to treat COPD, can increase renal potassium excretion
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Answer: ECG changes include flattening and inversion of T waves in mild hypokalemia, followed by Q-T interval prolongation, visible U wave and mild ST depression4 in more severe hypokalemia. Severe hypokalemia can also result in arrhythmias such as Torsades de points and ventricular tachycardia.
D) Link to patient details:
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Answer : If you’ve had a stroke, you have an increased risk for having a seizure. A stroke causes your brain to become injured. The injury to your brain results in the formation of scar tissue, which affects the electrical activity in your brain. Disrupting the electrical activity can cause you to have a seizure.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Answer : Abnormal increased activity in fronto-parietal association cortex and related subcortical structures is associated with loss of consciousness in generalized seizures. Abnormal decreased activity in these same networks may cause loss of conscious-ness in complex partial seizures. Thus, abnormally increased or decreased activity in the same networks can cause loss of consciousness. Information flow during normal conscious processing may require a dynamic balance between these two extremes of excitation and inhibition.
E) Link to patient details:
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Answer: By the history, Patient is an alcoholic and he has change in his gait since a year are the findings which leads to cause of ataxia.
Mechanism:Damage from alcohol is a common cause ofcerebellar ataxia. In patients with alcohol related ataxia, the symptoms affect gait (walking) and lower limbs more than arms and speech. It can also cause associated signs of peripheral neuropathy. Peripheral neuropathy is damage to the body's peripheral nervous system.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Answer :Patient has a history of binge drinking for 3 hours before the day of admission.
Heavy drinkers were about 1.6 times more likely to suffer from intracerebral hemorrhage and 1.8 times more likely to suffer from subarachnoid hemorrhage. The association between heavy alcohol consumption and these two types of stroke was stronger than that for ischemic stroke. Yes alchol could have increased IC bleeding.Liver damage due to too much alcohol can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain.
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
Answer: Yes
2.What are warning signs of CVA?
Answer: The five warning signs of stroke are:
•Sudden onset of weakness or numbness on one side of the body.
Sudden speech difficulty or confusion.
Sudden difficulty seeing in one or both eyes.
Sudden onset of dizziness, trouble walking or loss of balance.
Sudden, severe headache with no known cause.
3.What is the drug rationale in CVA?
Answer: DRUG RATIONALE FOR STROKE:
TREATMENT:
1.Injection Mannitol 100ml/IV/TD
Brain swelling is due to a cytotoxic reaction mediated by multiple factors, including free radicals.Brain swelling typically occurs in patients who have had an occlusion of the stem of the middle cerebral artery (MCA), and usually peaks at 3–5 days after stroke.
Mannitol is an osmotic diuretic, typically used at 0.25–0.5 g/kg IV administered over 15 minutes. It lowers intracranial pressure, and can be given every 6 hours.
2.TAB Ecospirin 75 mg po/OD:
Aspirin irreversibly inhibits cyclooxygenase, which prevents the conversion of arachidonic acid to thromboxane A2 (TXA2). Thromboxane A2 is a vasoconstrictor and stimulator of platelet aggregration. Platelets are inhibited for their full life cycle (5–7 days) after exposure to aspirin. Aspirin also inhibits prostacyclin activity and this inhibits platelet aggregration.
3.TAB ATORVAS 40mg po/HS:For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina (chest pain) due to a blood clot.
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
4.BP/PR/TEMP/SP02 MONITORING (4th hourly)
5.RT FEEDS-100ml milk with protein powder(2nd hourly):
Enteral feeding tubes, a nasogastric tube (NGT) or percutaneous endoscopic gastrostomy (PEG), are commonly used to provide nutrition, hydration and essential medications to stroke patients who cannot swallow.
4. Does alcohol has any role in his attack?
Answer:When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.Therefore it cannot be evaluated without further details
5.Does his lipid profile has any role for his attack??
Answer :The inverse relationship between serum HDL-C and stroke risk . When taken together it seems clear that higher baseline levels of serum HDL-C lower the risk of subsequent ischemic stroke.
G) Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
Answer : A characteristic dysfunction of the hand has been observed in various cervical spinal disorders when there is involvement of the spinal cord. There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement. The characteristic nature of the signs permit the distinction between myelopathy and changes due to nerve root or peripheral nerve disorder. The clinical significance of these signs has been assessed against other tests and their value in management is discussed.
2)What is finger escape ?
Answer :
All patients exhibited myelopathy hand, which was defined by two specific signs: the finger escape sign and the inability to grip and release rapidly with the fingers. Fourteen 3-mm micro-reflective markers were placed on the dorsal surface of the thumb and the index finger, and on the dorsal hand.
3)What is Hoffman’s reflex?
Answer :Hoffmann's reflex is a neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from the corticospinal tract.
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ? Answer: Thrombosis and infarction
2) What are the risk factors for cortical vein thrombosis?
Answer: Chronic Hemolytic anemias
Beta thalassemia
Heart diseases
Iron deficiency
Head trauma and injuries
Cancer
Intracranial hypotension
IBD and crohns disease
3)There was seizure free period in between but again sudden episode of GTCS why? Resolved spontaneously why ?
Answer :The postictal state is the altered state of consciousness after an epileptic seizure. It usually lasts between 5 and 30 minutes, but sometimes longer in the case of larger or more severe seizures, and is characterized by drowsiness, confusion, nausea, hypertension, headache or migraine, and other disorienting symptoms
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Answer: Anticoagulants
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Answer: Despite the fact that HFrEF and HFpEF share many risk factors and co-morbidities, there are substantial differences in systemic inflammation, cardiac remodelling (endothelial function, hypertrophy, and cardiomyocyte cell death), and stiffness (fibrosis, titin, and calcium levels). HFrEF, mostly occurs in male patients and is the consequence of cardiomyocyte loss. In contrast, HFpEF is often diagnosed in elderly female patients, who suffer from (a cluster of) non-cardiac comorbidities, such as hypertension, T2DM, stroke, anaemia, pulmonary disease, liver disease, sleep apnoea, gout, and cancer. HFpEF is characterized by low-grade chronic systemic inflammation and capillary dysfunction, with consequential low-grade cardiac inflammation. However, as most studies are conducted on models of established HFpEF, studies during the disease onset are required to elucidate the common denominator underlying the associated complications for HFpEF. In HFrEF, systemic and cardiac inflammation are secondary to the causes of cardiomyocyte loss. Whereas in HFpEF endothelial dysfunction mainly precedes its progression, in HFrEF endothelial dysfunction may rather be the consequence. Depending on the stimulus, perivascular (metabolic risks in HFpEF), interstitial (e.g., aging, hypertension in both HFpEF and HFrEF), or replacement (e.g., MI in HFrEF) fibrosis occurs and is differentially managed between the two conditions. The increased left ventricular stiffness in HFpEF is caused by reduced Ca2+ signalling, titin modifications (isoform shifts towards the stiffer isoform and post-translational changes), and increased perivascular and interstitial fibrosis. In contrast, in HFrEF, titin isoform switching is less consistent, and more flexible isoforms even present in end-stage non-ischemic dilated cardiomyopathy, therefore left ventricular stiffness ranges from being unaffected, to increased, or even reduced.
2.Why haven't we done pericardiocenetis in this pateint?
Answer:It’s resolving : 2.07cms effusion at the time of admission -1.4mm at the time of discharge)
DM type 2 (since 1month)
So, No need of pericardiocentis.
3.What are the risk factors for development of heart failure in the patient?
Answer:
Risk factors
High blood pressure.
Coronary artery disease
Diabetes.
Some diabetic and hypertensive medications.
• age
4.What could be the cause for hypotension in this patient?
Answer:Decreased venous return cause decreased cardiac output which results in hypotension.
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
Answer: Alcoholic cardiomyopathy is a form of heart disease caused by alcohol abuse. Long-term alcohol abuse weakens and thins the heart muscle, affecting its ability to pump blood
high blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels
High blood pressure can strain your heart, damage blood vessels, and increase your risk of heart attack
Diseases in the kidneys can affect the heart. It is common for people with chronic kidney disease or end-stage kidney disease to develop heart disease, including heart attack or heart failure.
2.what is the reason for anaemia in this case?
Answer: When you have kidney disease, your kidneys cannot make enough EPO. Low EPO levels cause your red blood cell count to drop and anemia to develop. Most people with kidney disease will develop anemia. Anemia can happen early in the course of kidney disease and grow worse as kidneys fail and can no longer make EPO
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Answer: Diabetes mellitus
4. What sequence of stages of diabetes has been noted in this patient?
Answer: stage 1: defined as DCBD (dysglycemia-based chronic disease )insulin resistance;
stage 2: defined as DCBD prediabetes;
stage 3: defined as DCBD type 2 diabetes; and
stage 4: defined as DCBD vascular complications, including retinopathy, nephropathy or neuropathy, and/or type 2 diabetes-related microvascular events.
All these stages have been noted in this case
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :Patient was apparently asymptomatic 2 days ago when he developed Shortness of breath Grade II (on exertion) which progressed to Grade IV (at rest) for which he visited local RMP and was referred to our hospital.Patient also complains of decreased urine output since 2 days and Anuria since morning.
Anatomical localization is heart
Primary etiology is atrial fibrillation
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:) INJ. Dobutamine 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg.
Mechanism of action: Dobutamine is a direct-acting inotropic agent whose primary activity results from stimulation of the ß receptors of the heart while producing comparatively mild chronotropic, hypertensive, arrhythmogenic, and vasodilative effects. It does not cause the release of endogenous norepinephrine, as does dopamine
2) TAB. Digoxin 0.25mg OD 5/7 and INJ. Unfractionated Heparin 5000 IU TID.
Mechanism of action: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication: Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the hear.
3[INJ. Unfractionated Heparin Infusion @5ml/hr
Mechanism of action: It produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism. ... By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin-induced activation of platelets and of factors V and VIII.Other medications used during the course in hospital -
1. TAB. Cardivas3.125mg PO/BD
2. TAB. Dytor 10mg PO/OD
3. TAB Pan D 40mg PO/OD
4. TAB. Taxim 200mg PO/OD
5. INJ. Thiamine 100mg in 50ml NS IV/TID
6. INJ. HAI S.C 8U-8U-6U
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Answer: The pathophysiology of CRS can be attributed to two broad categories of "hemodynamic factors" such as low cardiac output, elevation of both intra-abdominal and central venous pressures, and non-hemodynamic factors or "cardiorenal connectors" such as neurohormonal and inflammatory activation.[5] It was previously believed that low cardiac output in heart failure patients result in decreased blood flow to the kidneys which can lead to progressive deterioration of kidney function. As a result, diuresis of these patients will result in hypovolemia and pre-renal azotemia.
In addition, CRS has been observed in patients with diastolic dysfunction who have normal left ventricular systolic function.[3]Therefore, there must be additional mechanisms involved in the progression of CRS. Elevated intra-abdominal pressures resulting from ascites and abdominal wall edema may be associated with worsening kidney functions in heart failure patients. Several studies have shown that as a result of this increased intra-abdominal pressure there is increased central venous pressure and congestion of the kidneys' veins, which can lead to worsening kidney function.[3]
In addition, many neurohormonal and inflammatory agents are implicated in the progression of CRS. These include increased formation of reactive oxygen species, endothelin, arginine vasopressin, and excessive sympathetic activity which can result in myocardial hyprtrophy and necrosis.
Other cardiorenal connectors include renin-angiotensin-system activation, nitric oxide/reactive oxygen species imbalance, inflammatory factors and abnormal activation of the sympathetic nervous system, which can cause structural and functional abnormalities in both heart and/or the kidney. There is a close interaction within these cardiorenal connectors as well as between these factors and the hemodynamic factors which makes the study of CRS pathophysiology complicated.
4) What are the risk factors for atherosclerosis in this patient?
Answer:
High cholesterol and triglyceride levels.
High blood pressure.
Smoking.
Type 1 diabetes.
Obesity.
Physical inactivity.
High saturated fat diet.t?
5) Why was the patient asked to get those APTT, INR tests for review?
Answer:Standard coagulation screening tests such as activated partial thromboplastin time (APTT), prothrombin time (PT), and the international normalized ratio (INR) are important constituents of basic examinations in clinical laboratories. APTT can be used as an indicator of intrinsic coagulation pathway activity, and a short APTT is linked to increased thrombin generation and increased risk for thrombosis.
D) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :Evolution of symptomatology
12 years ago- DM2
1year back Heart burn like episodes(relieved without medication)
7 months back pulmonary TB (completed the course one month back)
6 months back Hypertension
1/2 hour ago- SOB
Anatomical localisation: Heart muscle
Primary etiology
Coronary artery disease:involves the reduction of blood flow to the heart muscle due to build-up of plaque (atherosclerosis) in the arteries of the heart
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:Met XL 25 tablet is used to lower the raised blood pressure and various other heart-related conditions such as angina (chest pain), heart failure, preventing further complications.
Glimiprime M 2 Forte Tablet is a combination of two medicines: Glimepiride and Metformin. This medicine is used in the treatment of type 2 diabetes mellitus (DM). It improves blood glucose levels in adults when taken along with proper diet and regular exercise
Telma 20 tablet is an antihypertensive medicine that is used to treat high blood pressure and can also help in reducing other heart problems It acts by relaxing the blood vessels and leads to lower blood pressure
3) What are the indications and contraindications for PCI?
Answer:Indications
The following are the clinical indications that could require a percutaneous coronary intervention.
Acute ST-elevation myocardial infarction (STEMI)
Primary PCI is the recommended method of reperfusion when it can be performed in a timely fashion by experienced operators.[1]
STEMI and ischemic symptoms of less than 12 hours' duration.[2]
STEMI and ischemic symptoms of less than 12 hours' duration and contraindications to fibrinolytic therapy
PCI improves survival in patients with significant (>50%) stenosis
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Early invasive therapy (within 2 hours of symptoms) recommended with refractory angina, recurrent angina, symptoms of heart failure, new or worsening mitral regurgitation, hemodynamic instability, or sustained ventricular tachycardia/fibrillation.
A worsening of troponin levels should trigger an early therapy (within 24 hours)
Unstable angina
Stable angina
Anginal equivalent (e.g., dyspnea, arrhythmia, or dizziness or syncope)
High-risk stress test findings
PCI is indicated for the critical coronary artery stenosis, which does not qualify for coronary artery bypass surgery (CABG).[3]
Contraindications
Absolute Contraindications:
Noncompliance with the procedure and inability to take dual antiplatelet therapy.
High bleeding risk (thrombocytopenia, peptic ulcer, severe coagulopathy)
Multiple percutaneous coronary intervention restenosis
Relative Contraindications:
Intolerance for oral antiplatelets long-term
Absence of cardiac surgery backup
Hypercoagulable state
High-grade chronic kidney disease
Chronic total occlusion of SVG
An artery with a diameter of <1.5 mm
Stenosis of <50%
Critical left main stenosis with no collateral flow or patent bypass graft
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Answer: Overtreatment refer to the detection and treatment of conditions that would not ultimately affect an individual's health. With increasing detection of small renal masses there is growing awareness of the overdiagnosis and overtreatment of these tumors, supported by studies showing that 15-30% of nephrectomy specimens are pathologically benign, and that many small renal cell carcinomas are indolent. The harms of overdiagnosis and overtreatment are numerous, including psychosocial stressors and renal morbidity, in addition to unnecessary surgical complications. A greater understanding of the potential harms of overdiagnosis and overtreatment is crucial as clinicians focus on optimizing patient selection for renal mass biopsy, active surveillance protocols, and minimally invasive surgery.
Overdiagnosis is the diagnosis of an abnormality that bears no substantial health hazard and no benefit for patients to be aware of. Resulting mainly from the use of increasingly sensitive screening and diagnostic tests, as well as broadened definitions of conditions requiring an intervention, overdiagnosis is a growing but still largely misunderstood public health issue. Fear of missing a diagnosis or of litigation, financial incentives or patient’s need of reassurance are further causes of overdiagnosis. The main consequence of overdiagnosis is overtreatment. Treating an overdiagnosed condition bears no benefit but can cause harms and generates costs. Overtreatment also diverts health professionals from caring for those most severely ill. Recognition of overdiagnosis due to screening is challenging since it is rarely identifiable at the individual level and difficult to quantify precisely at the population level. Overdiagnosis exists even for screening of proven efficacy and efficiency. Measures to reduce overdiagnosis due to screening include heightened sensitization of health professionals and patients, active surveillance and deferred treatment until early signs of disease progression and prognosis estimation through biomarkers (including molecular) profiling. Targeted screening and balanced information on its risk and benefits would also help limit overdiagnosis. Research is needed to assess the public health burden and implications of overdiagnosis due to screening activity.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:Evolution of symptomatology:
Uncontrolled DM2 since 8 years
3 days back Mild chest pain dragging type and retrosternal pain(radiated)
Anatomical localisation: Inferior wall of heart
Primary etiology: Diabetes type 2 (uncontrolled)
high blood glucose from diabetes can damage your blood vessels and the nerves that control your heart and blood vessels
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:TAB. ASPIRIN 325 mg PO/STAT
Mechanism of action: The acetyl group of acetylsalicylic acid binds with a serine residue of the cyclooxygenase-1 (COX-1) enzyme, leading to irreversible inhibition. This prevents the production of pain-causing prostaglandins.
TAB ATORVAS 80mg PO/STAT
Mechanism of action: Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
TAB CLOPIBB 300mg PO/STAT
Mechanism of action: The active metabolite of clopidogrelselectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
INJ HAI 6U/IV STAT
VITAL MONITORING.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Answer:Repeat PTCA provides a valuable, safe and cost-effective way of management for recurrence of stenosis after initially successful angioplasty. It increased the percent of patients with documented long-term success of angioplasty
Over testing and over treatment can raise a person’s risk of cardiovascular death by as much as four times.
F) Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Answer: Fluids and plasma are given through an IV. Medications to treat cardiogenic shock are given to increase your heart's pumping ability and reduce the risk of blood clots.
2. What is the rationale of using torsemide in this patient?
Answer:Torsemide is an antihypertensive diuretic causes decrease in blood pressure, here patient is already hypotensive, then what is the need to give this torsemide and decrease the BP further
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Answer:for the treatment of UTI (white discharge)
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer: Evolution of symptomatology:
Patient having no comorbidities who is a an alcoholic saying history of pain abdomen and vomitings 5 years back
Got treated for it and stopped alcohol consumption for 3 years. In that three years he is well
Again he started alcohol consumption .
Recurrence of pain abdomen and vomitings
Recurrent episodes of 5 to 6 in last year are treated by local rural medical practitioner
Increased the alcohol intake in last 20 days
Last alcohol intake was 1 week back
Pain abdomen and vomitings reccured
Also associated with constipation.fever with chills and rigor, burning micturition
Abdominal pain is in umbilical,hypogastric,left lumbar, and left hypochondrium
Anatomical localization : left upper quadrant of abdomen
Primary etiology : alcohol aggravated pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer:) ING. MEROPENAM ; TID for 7 days
* Meropenem ( broad spectrum Carbepenem ) an antibiotic.
2) ING. METROGYL 500 mg IV TID for 5 days
* inj. Metrogyl has METRONIDAZOLE
( Nitroimidazole drug ) an antibiotic
3) ING. AMIKACIN 500 mg IV BD for 5days
* It is an Aminoglycoside antibiotic
## Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
4) TPN ( Total Parenteral Nutrition )
* Method of feeding that by passes gastrointestinal tract
* Fluids are given to vein , it provides most of the nutrients body needs.
* TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
* Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD
* Inj. Pantop has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD
* It is an opioid analgesic, given to releive pain
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Answer:Ascites
Ascites elevates the diaphragms and causes basilar atelectasis, which contributes to dyspnea and mild hypoxia. Some patients with ascites have diaphragmatic defects that allow ascites fluid to flow into the chest, causing a pleural effusion termed a hydrothorax.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Answer:Pancreatitis results in damage to beta cells. Results in decreased insulin and hyperglycemia
This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress or the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
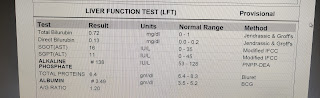
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Answer: The most common causes of acute pancreatitis are gallstones and alcohol-induced pancreatitis. This patientss liver enzymes (especially ALT) and bilirubin level are elevated, which may suggest choledo- cholithiasis.
The biochemical markers of a biliary etiology of acute pancreatitis (AP) include an ALT elevation of more than 3 times the upper range of normal (ULN) and a serum total bilirubin greater than 3 mg%
4) What is the line of treatment in this patient?
Answer: IVF: 125 mL/hr - to maintain body fluids and volumes
• Inj PAN 40mg i.v OD - antacids for gut protection
• Inj ZOFER 4mg i.v sos- antiemetic for nausea and vomiting
• Inj Tramadol 1 amp in 100 mL NS, i.v sos- narcotic analgesic for pain relief
• Tab Dolo 650mg sos - NSAID for pain
• GRBS charting 6th hourly
• BP charting 8th hourly
For the master chart to the "pancreatitis thesis project" please get in touch with Dr Shashikala PGY1 and Dr Divya PGY2 and share their insights into the above project problem they are working on.
C) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
Answer: Ruptured liver abscess
2) What was the cause of her death?
Answer:
* May be SEPSIS with MODSdue to ruptured liver abcess…
# But again etiology ; can be confirmed only by exploratory laporotomy
3) Does her NSAID abuse have something to do with her condition? How?
Answer:NSAIDS are known to cause drug induced hepatitis which may lead to cirrhosis.
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
Answer:due to Acidosis which was caused by Diuretics
2. Why does he have intermittent episodes of drowsiness ?
Answer:
3. Why did he complaint of fleshy mass like passage in his urine?
Answer:plenty of pus cells in his urine passage appeared asfleshy mass like passage to him
4. What are the complications of TURP that he may have had?
Answer:Difficulty micturition
Electrolyte imbalances
Infection
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
Answer :Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
Answer: Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
Answer:bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Answer: History findings:
Cough
Difficulty in swallowing to solids and eventually to liquids too
Hoarseness of voice
Inadequate sleep
Examination findings:
Wheezing
Positive laryngeal crepitus
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Answer: Paradoxical C-IRIS is reported to occur in 13%–45% of HIV-infected persons who start ART after treatment for CM.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?what could be the cause in this patient ?
Answer: it was undoubtedly proved that alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Answer:Alcohol changes gut permeability, increasing absorption of endotoxins released by bacteria in the gut. In response to the endotoxins (which the impaired liver can no longer detoxify), liver macrophages (Kupffer cells) release free radicals, increasing oxidative damage.
3. Is liver abscess more common in right lobe ?
Answer:50% of solitary liver abscesses occur in the right lobe of the liver (a more significant part with more blood supply), less commonly in the left liver lobe or caudate lobe
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Answer:Ultrasound guided percutaneous drainage is one form of image guided procedure, allowing minimally invasive treatment of collections that are accessible by ultrasound study.
Indications for percutaneous drainage are broad: essentially any abnormal fluid collection in the patient which can be accessible. Examples include:
complicated diverticular abscess
Crohn's disease related abscess
complicated appendicitis with appendicular abscess
tuboovarian abscess
post-surgical fluid collections
hepatic abscess (e.g. amoebic or post-operative)
renal abscess or retroperitoneal abscess
splenic abscess
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
Answer:Amoebic or pyogenic infection
2) How do you approach this patient ?
Answer: proper history
Suitable investigations
Radiological assessment
Medications against amoeba and bacteria
Usg guided drainage after liquifaction of abscess
If unresolved, surgical treatment.
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
Answer: To prevent the secondary bacterial infections in amoebic liver abscess and also we cannot take risk until we confirm it as amoebic
Hence we need to administer antibiotics too
4) Is there a way to confirmthe definitive diagnosis in this patient?
Answer: Ultrasound abdomen followed by CT scan and blood tests
Amoebic specific tests
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:Patient is a known hypertensive from past 3 years.
He went for covid 19 vaccination and from that night he's complaining of fever with chills and rigor.
Facial puffiness amd periorbital edema after 10 days of vaccination
Theb afterwards he developed weakness in right upper amd lower limb.
Then after one week , he presented with altered sensorium
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer:LIPOSOMAL AMPHOTERICIN B and ITRACONAZOLE
Antifungals to be given in mycosis caused by mucor, rhizopus etc
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Answer: Mucormycosis, colloquially known as black fungus, is a serious fungal infection that was seen in far smaller numbers in India before Covid-19, too. But it is now affecting post-Covid patients in large numbers. As of May 22, the government has reported 8,848 cases of this fungal disease, which can lead to serious complications and has a high rate of mortality.
Thus far, this surge has been attributed to the improper use of steroids to treat Covid-19 patients, coupled with poorly managed diabetes. But steroids in themselves are not the villains.
“Systemic (oral and intravenous) corticosteroids have been proven to reduce mortality in Covid-19,” Lancelot Pinto, consultant pulmonologist at Mumbai’s Hinduja Hospital, told Quartz. “The largest trial, Recovery, which proved this beyond a reasonable doubt among individuals who had low oxygen levels, used them in a dose of 6 milligrams Dexa per day for up to 10 days.”
Not only in Covid-19, but steroids are also widely used in orthopaedic and pulmonary diseases. In India, the problem lies not in the drug but in how it is prescribed. “Most of us who work in India will agree that prescribing practices more often than not tend towards higher doses for longer periods of time, which is a clear risk factor for invasive fungal infections,” Pinto said. Added to this, there is no strict prescription check in India, and most drugs—even those that need a prescription—can be easily bought over-the-counter.
“In addition, India has an epidemic of type 2 diabetes, and a significant proportion of patients with diabetes are diagnosed late in the illness,” which, according to Pinto, could be contributing to this surge in cases.
9) Infectious Disease (Covid 19)
1) Covid 19 with co morbidity
Possible questions:
1) How does the pre-existing ILD determine the prognosis of this patient?
Answer: The prognosis in this patient worsens , as the patient of this condition has poor lung reserve and impaired gas exchange and they are often on immunosuppressive therapy , that increases the chances of multiple co morbidities and at constant risk of acute exacerbations.
2) Given the history of autoimmune disease in the patient, how does the administration of steroids for COVID affect her RA and hypothyroidism?
Answer:
3) Would this patient have an increased risk for post covid autoimmune response compared to patients without a history of autoimmune disease?
Answer: yes
4) Why was she prescribed clexane (enoxaparin)?
Answer: Clexane is an ANTI COAGULANT ,here she was prescribed with it because covid 19 may lead to hyper coagulable state. According to some invitro studies ,it is shown that there is increased gene expression of FGF, FGG and SERPIN leading to upregulation of coagulation cascade factors including factor 2,3 ,10 ultimately leading to procoagulable state .
2) Covid 19 with Diabetes
Link to the patient case report log:
Questions:
1) Since patient didn't show any previous characteristic diabetes signs, did the Covid-19 infection aggravate any underlying condition and cause the indolent diabetes to express itself? If so what could be the biochemical pathways that make it plausible?
Answer: The patient may be prediabetic ,the acute inflammation and steroid treatment may push them into having diabetes.for example, the mild stressors like overweight(not obese ),mild sedentary life style and the insulin resistance developed from acute infection and steroids used for the covid treatment leads to the significant increase in the insulin production, required to keep glucose levels normal but the pancreas wasn't able to increase the output to that level. As the human pancreas expresses the ACE2,virus might enter islets and causes acute beta cell dysfunction leading acute hyperglycemia and transient Type2DM.
2) Did the patient's diabetic condition influence the progression of her pneumonia?
Answer: Yes, the Diabetic condition may increase the susceptibility to pneumonia for several reasons ,like decreased immunity (as the hyperglycemic state can weaken person's immune system defenses), impaired Lung function , pulmonary microangiopathy ,increased risk of aspiration in diabetic patients etc .
3) What is the role of D Dimer in the monitoring of covid? Does it change management or would be considered overtesting?
Answer : D-dimers are characteristically released as degeneration products of cross linked fibrin during plasma coagulation; the increased levels of D-dimer indicate the activation of coagulation ,as in Covid condition ,hypercoagulable state may be present. It is not over testing ,as it indicates coagulability state , we can manage it, by monitoring the increased D-dimer level by prescribing anti coagulants.
3) Covid 19 Severe
Link to the complete case report log:
Questions:
1. Why was this patient given noradrenaline?
Answer : Noradrenaline preferentially stimulates α1-adrenoceptors on peripheral vessels leading to marked vasoconstriction, it is given as the patient had hypotension along with AKI .
2. What is the reason behind testing for LDH levels in this patient?
Answer :It is most active in the liver, striated muscles, heart, kidneys, lungs, brain, and red blood cells (erythrocytes). In the case of cell damage, lactate dehydrogenase is released from inside them, its concentration and activity in the blood increase. High serum LDH activity is a negative prognostic factor in such patients.
3. What is the reason for switching from BiPAP to mechanical ventilation with intubation in this patient? What advantages did it provide?
Answer : BiPAP is a non invasive type of mechanical ventilation ,where delivery of Oxygen is done through facial mask ,it works by creating positive airway pressure ,that is the pressure outside is greater than the pressure in lungs .
In invasive type of mechanical ventilation ,tube is inserted which is called tracheal intubation. It is more effective as the patient doesn't need to work as hard as to breathe ,their respiratory muscles are at rest .Helps the patient to get adequate oxygen
and clears carbondioxide .Patient is allowed time to recover in hopes that breathing becomes normal again .
4) Covid 19 Mild
Link to the case report log:
Questions:
1. Is the elevated esr due to covid related inflammation?
Answer: Yes ,can say ,it is due to Covid. As it is observed in many of the patients ,who got infected with covid.
2. What was the reason for this patient's admission with mild covid? What are the challenges in home isolation and harms of hospitalization?
Answer: Here the patient had developed SOB even after taking treatment and home isolation.Though its a mild covid ,duration of disease is longer(more than 14 days of home isolation ,not recovered) and patients usually get panic over these things and mainly SOB affects mental stability too .
Challenges in home isolation are; to maintain social distance from our beloved ones ,and get isolated in a proper ventilated room , following treatment provided by doctor and some of home remedies may be useful, physicalexercise ,staying positive etc.
Harms of hospitalization may include cross infections , hospital acquired infections and also iatrogenic infections.
5) Covid 19 and comorbidity (Altered sensorium, azotemia, hypokalemia)
Link to the case report log:
Questions:
1) What was the reason for coma in this patient?
Answer: Prolonged unconscious state following covid infection may lead to coma in some patients .
Answer:severe hypoxia
2) What were the competency gaps in hospital 1 Team to manage this intubated comatose patient that he had to be sent to hospital 2? Why and how did hospital 2 make a diagnosis of hypokalemic periodic paralysis? Was the coma related?
Answer: Here in hospital 2 ,we have observed acute flaccid paralysis in patient ,on investigations it is releaved decreased potassium levels; hypokalemic periodic paralysis is a genetic disorder of autosomal dominant inheritance ,
3) How may covid 19 cause coma?
Answer : prolonged unconsciousness state may lead to coma in some patients
6) Severe Covid 19 with altered sensorium
Link to the case report log:
1. What was the cause of his altered sensorium?
Answer: ICU psychosis aggravated by alcohol withdrawal
2. What was the cause of death in this patient?
Answer: cardiopulmonary arrest
7) Covid 19 Moderate with ICU psychosis
Link to the case report log:
Questions :
What is the grade of pneumonia in her?
Answer: There is no requirement in knowing grade of pneumonia in patient ,take into consideration corad score and ct value ,5 and 12 value respectively shows it as moderate condition .
What is the ideal day to start steroids in a patient with mild elevated serum markers for COVID ?
Answer: the anti inflammatory steroid should be initiate early in the pulmonary phase to counter the immune dysregualtion .
Ideal time for steroid initiation ;is after 8th day of symptoms ,when virus is very low replicable ,and inflammatory response is about to settle down .if steroids. Are started in the early viral replicable phase ;there is chance that the virus replicates more .
What all could be the factors that led to psychosis in her ?
Answer: ICU
In what ways shall the two drugs prescribed to her for psychosis help ?
Answer : resperidone, in low doses ,given for ICU psychotic patients and useful in delirium.
Second drug is Piracetam ; under pharmacological classification falls under Nootropics with properties of memory and cognitive enhancement .
It is said to improve mood and motivate the mind.
Being a derivative of Gamma aminobutyric acid , it modulates neurotramission in a range of transmitter systems ( proportion of GABAergic and cholinergic tranmission )
It has neuroprotective and anticonvulsant properties
It enhances neuroplasticity
What all are the other means to manage such a case of psychosis?
Answer:
- correct underlying diseases
- good sleep
- anti psychotic therapy
What all should the patient and their attendants be careful about ( w.r.t. COVID )after the patient is discharged ?
Answer : inflammatory markers
What are the chances that this patient may go into long covid given that her "D Dimer" didn't come down during discharge?
Answer :
long covid - increased CRP AND D -DIMERS
This patient has elevted D -DIMERS at discharge, so she has a potential risk to go into long covid
8) Covid 19 Moderate
Link to the complete case report log
Questions:
1. Can psoriasis be a risk factor for severe form of COVID?
Answer:
No
2. Can the increased use of immunomodulatory therapies cause further complications in the survivors?
Answer:YES, these drugs aim at reducing immune responese by supressing immue system
*this may actually lead to funagl infections like mucormycosis in a survivor
3. Is mechanical ventilation a risk factor for worsened fibroproliferative response in COVID survivors?
Answer:
Third risk factor is prolonged ICU stay and duration of mechanical ventilation. While disease severity is closely related to the length of ICU stay, mechanical ventilation poses an additional risk of ventilator-induced lung injury (VILI). Abnormalities of pressure or volume settings underlie this injury leading to a release of proinflammatory modulators, worsening acute lung injury, and increased mortality or pulmonary fibrosis in survivors
9) Covid with de novo Diabetes
Link to Case report log:
•What is the type of DM the patient has developed ?(is it the incidental finding of type 2 DM or virus induced type 1DM )?
Answer:cannot be determined
•Could it be steroid induced Diabetes in this patient?
Answer:yes
10) Comparing two covid patients with variable recovery
What are the known factors driving early recovery in covid?
Answer:
young age
*controlled sugars
*asymptomatic infection
*no comorbidities
11) Covid moderate with first time detected diabetes:
Link to Case report log :
Questions-
1) How is the diabetes related to the prognosis of COVID patients? What are the factors precipitating diabetes in a patient developing both covid as well as Diabetes for the first time?
Answer:
prognosis is worsened due to diabtes
covid causes pancreatic damage through ACE2 receptors which may lead to DENOVO DIABETES
2) Why couldn't the treating team start her on oral hypoglycemics earlier?
Answer:
- insulin is more effective in bringing back the sugar levels.
- so she was not started on oral drugs
12) Moderate to severe covid with prolonged hospital stay:
Questions :-
1) What are the potential bioclinical markers in this patient that may have predicted the prolonged course of her illness?
Answer:
13) Severe covid with first diabetes
Link to Case report log :
What are the consequences of uncontrolled hyperglycemia in covid patients?
Answer:
Does the significant rise in LDH suggests multiple organ failure?
Answer:
What is the cause of death in this case?
Answer:
14) Long covid with sleep deprivation and ICU psychosis
Link to Case report log:
Questions:
1)Which subtype of ICU psychosis did the patient land into according to his symptoms?
Answer:
2)What are the risk factors in the patient that has driven this case more towards ICU pyschosis?
Answer:
3)The patient is sleep deprived during his hospital stay..Which do u think might be the most propable condition?
A) Sleep deprivation causing ICU pyschosis
B) ICU psychosis causing sleep deprivation
Answer:
4) What are the drivers toward current persistent hypoxia and long covid in this patient?
Answer:
15) Moderate Covid with comorbidity (Trunkal obesity and recent hyperglycemia)
Link to Case report Log:
QUESTIONS:
1. As the patient is a non- diabetic, can the use of steroids cause transient rise in blood glucose?
Answer : Yes
2. If yes, can this transient rise lead to long term complication of New-onset diabetes mellitus?
Answer:MAY BE
It depends on other risk factors of DM
As of now glycated Hb is high normal
It means that patient has high sugars even before the covid infection.
as he is already predisposed to have DM
THERE IS A HIGH CHANCE OF DEVELOPING DM
3. How can this adversely affect the prognosis of the patient?
Answer:HYPERGLYCEMIA based on its extent worsens the prognosis.
4. How can this transient hyperglycemia be treated to avoid complications and bad prognosis?
Answer: Basing on the above cited source, the patients with significant rise in glucose must be treated
# those with glucose levels less than 200 mg/dl can use oral hypoglycaemics\
# severe covid|+high sugars= insulin
5. What is thrombophlebitis fever?
Answer:
fever in thrombophlebitis due to inflammatory response
6. Should the infusion be stopped inorder to control the infusion thrombophlebitis? What are the alternatives?
Answer:
STOPPING INFUSION is not needed
DOC: NSAID
16) Mild to moderate covid with hyperglycemia
QUESTIONS:
1. What could be the possible factors implicated in elevated glycated HB ( HBA1c ) levels in a previously Non-Diabetic covid patient?
Answer : COVID 19 is known to cause pancreatic islet cells as it have more receptor expression in endocrine pancreas. this might have led to deficiency of insulin in a previously susceptible patients with impaired glucose tolerance
2. What is the frequency of this phenomenon of New Onset Diabetes in Covid Patients and is it classical type 1 or type 2 or a new type?
Answer:As the covid 19 infection causes extensive pancreatic damage it may lead to insulin deficiency.Further, insulin resistance is also implicated due to IL-6 ,TNF -alpha etc..,there is a high propensity to cause diabetes in post -COVID state
3. How is the prognosis in such patients?
Answer:Diabetes is a hypercoaguable state. NEW ONSET DM has more severe effect. There is a higher propensity of thrombotic events via ANTI THROMBIN 3 mediated mechanism.
THIS IS ALL LEADING TO A WORST PROGNOSIS IN THIS PATIENT
4. Do the alterations in glucose metabolism that occur with a sudden onset in severe Covid-19 persist or remit when the infection resolves?
Answer:
depends upon the patients existing health status.
5) Why didn't we start him on Oral hypoglycemic agents earlier?
Answer:
17) Covid 19 with hypertension comorbidity
1)Does hypertension have any effect to do with the severity of the covid infection.If it is, Then how?
Answer:
- YES, HYPERTENSION IS ASSOCIATED WITH WEAK IMMUNE SYSTEM THEREBY GREATER SEVERITY
2)what is the cause for pleural effusion to occur??
Answer: pneumonia
18) Covid 19 with mild hypoalbuminemia
QUESTIONS:
1. What is the reason for hypoalbuminemia in the patient?
Answer:
- DECREASED SYNTHESIS
- INCREASED METABOLISM
2. What could be the reason for exanthem on arms? Could it be due to covid-19 infection ?
Answer:
- It is generally seen in viral infections and therefore can be due to covid infection
3. What is the reason for Cardiomegaly?
Answer:
uncrontrolled hypertension ....
4. What other differential diagnoses could be drawn if the patient tested negative for covid infection?
Answer:
5. Why is there elevated D-Dimer in covid infection? What other conditions show D-dimer elevation?
Answer:
Covid 19 is a hypercoaguable state. In the later stages of diseases, thrombosis may set in .
D-Dimers are suggestive of thrombotic events
20) Covid 19 with first time diabetes
Questions:
1)Can usage of steroids in diabetic Covid patients increases death rate because of the adverse effects of steroids???
Answer :There is no clear cut evidence that steroids definitely increase mortality in diabetic covid patients.But due to a potential risk OTHER ALTERNATIVE should be first choice rather than a steroid.
But, when steroids are used ,they must be cautiously used . A patient on oral hypoglycemic drugs must always be shifted to insulin therapy.
2)Why many COVID patients are dying because of stroke though blood thinners are given prophylactically???
Answer :
3)Does chronic alcoholism have effect on the out come of Covid infection????
If yes,how??
Answer:
21) Severe Covid with Diabetes
Questions-
1. What can be the causes of early progression and aggressive disease(Covid) among diabetics when compared to non diabetics?
Answer : DIABETES is a chronic inflammatory condition which alters our metabolic state and thereby intervening in our body's response to pathogenic organisms.DIABETES SPECIFICALLY TYPE 2, characterised by hyperglycemia and insulin resistance would promote the production of glycosylation end products and pro inflammatory cytokines. In addition to this, it also promotes the production of adhesive molecules which are a key in tissue inflammation.
This may be the basic pathogenesis which not only increases the susceptibility of an individual to infections but also increases the severity.
2. In a patient with diabetes and steroid use what treatment regimen would improve the chances of recovery?
Answer:
Glycemic control : with insulin or oral agents
limited usage of steroids
careful monitoring of patient
oxygenation if needed
3. What effect does a history of CVA have on COVID prognosis?
Answer:As per the study conducted , there is an increased risk of mortality and morbidity in patients with prior history of stroke
23) Covid 19 with multiple comorbidities:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-viral-pneumonia.html
1) What do you think are the factors in this patient that are contributing to his increased severity of symptoms and infection?
Answer : Preexisting lung disease inform of tuberculosis and bronchial asthma
diabetes mellitus
prior attack of pneumonia
CKD
2) Can you explain why the D dimer levels are increasing in this patient?
Answer:COVID &DM are both hypercoaguable states
this might have initiated the thrombosis in the patient which is marked by rise in D-DIMER levels
3) What were the treatment options taken up with falling oxygen saturation?
Answer:Head end elevation
*Continuous O2 inhalation
*Intermittent BiPaP
* Bronchodilators
4) Can you think of an appropriate explanation as to why the patient has developed CKD, 2 years ago? (Note: Despite being on anti diabetic medication, there was no regular monitoring of blood sugar levels and hence no way to know for sure if it was being controlled or not)
Answer :
10. MEDICAL EDUCATION:
.
10) Medical Education: (10 marks)
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home: https://onedrive.live.com/view.aspx?resid=4EF578BAE67BA469!4180&ithint=file%2cdocx&authkey=!AOy7BpRTn42DBMo


Comments
Post a Comment