66 YEARS OLD MALE WITH ASCITES
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
Name : K. Supriya (9th semester)
Roll number : 53
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
66 YEARS OLD MALE PATIENT FROM JAGATPALLY ,TODDY CLIMBER BY OCCUPATION,CAME TO OPD WITH THE FOLLOWING
Presenting complaints :
Abdominal distension since 1 and half month
Nausea and decreased appetite since 1 and half month
Decreased urine output since 10 days
Constipation since 2 days
This 66 yr old male patient ,who is deaf and dum since birth have very good relationships with family ,which includes his wife ,3 daughters and 1 son .He is toddy tree climber by occupation .He was regular to his work since 2yrs ago and active person ,who used to wake up at 4:30 am and have tea in the morning and goes to his work and used to have lunch at 10:30 am (rice & curry) and at around 3:30 pm ,he used to have food again (rice & curry )as he goes to work after that ,he used to take tea in the evng and at around 9:00 pm ,dinner (rice&curry)
He stopped work 2yrs ago ,from then ,he wakes up at 6:00 and have food at 10 :30 am and stopped eating at around 3:30 in the afternoon , remaining everything is asusual as before .
He diet is of mixed type ,occasional alcoholic and Gutkha chewer .
HOPI :
Patient was apparently assymptomatic 2 years ago ,then he noticed swelling ,which was sudden in onset and rapidly progressive for which he was operated within 4 days of onset in choutuppal .
Now ,he came to OPD as he noticed abdominal distension after intake of food ,associated with nausea ,pain abdomen at epigastric region.
So ,he reduced his daily intake of food .
Patient attenders noticed that he is reducing body weight .
Decreased urine output since 10 days
Difficulty in passing stools since 2days and passing flatus .
B/L swelling of lower limbs upto ankle region ,which is of pitting type .
No H/O facial puffiness ,Shortness of breath , palpitations ,fever ,cough .
H/O fall from tree while climbing 5years ago .
Past History :
Not a known case of diabetes , Hypertension ,Asthma , epilepsy ,TB ,CAD
Personal History :
Appetite : Decreased
Diet : Mixed
Bowel and bladder movements : Decreased urine output and constipation present
addictions : occasional alcoholic ,Gutkha chewer ,non smoker
allergies : No allergies
General Examination :
Patient is Conscious , Coherent and Co operative
Moderately Built and Moderately Nourished .
Pallor -present
Icterus , Cyanosis ,clubbing , lymphadenopathy - absent
Vitals :
Temperature : afebrile
Pulse rate : 98 bpm
Respiratory rate : 16 cpm
Blood pressure : 120 /70 mm Hg
SpO2 :98 % at room temperature
Systemic Examination :
Per abdomen:
Shape of the abdomen : distended
Umblicus : everted or slit shaped
Tenderness present at epigastric and right lumbar region .
Fluid thrill : present
Bowel sounds: present n heard
No engorged veins and visible pulsations
CVS :
S1 ,S2 heard
JVP : Normal
RS:
Bilateral Air Entry : present
Vescicular breath sounds heard
No crepts
CNS :
Higher mental functions : intact
Provisional diagnosis : Peritonitis ?
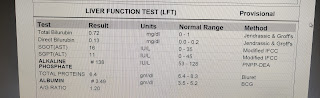
Investigations :
Ascitic tap done
Cytology report :
SAAG : 0.5
Sugars :78
Protein : 3.9
Cell count : Tc - 1155 (corrected WBC count )
Dc - 80% lymphocytes ,20% neutrophils.
Low SAAG with Lymphocytic predominance .
Treatment :
1. FLUID RESTRICTION 1.5-2LIT/DAY
2. INJ. CEFOTOXIME 1g/ IV/PV
3. TAB. LASIX 40mg/PO/BD
4. SYRUP. LACTULOSE 15ml/PO/BD
5. TWO EGG WHITES / DAY
6. PROTEIN X POWDER 2 SCOOPS IN 100ml BD
7. DAILY BODYWEIGHT AND ABDOMINAL GIRTH
8. STRICT INPUT/OUTPUT CHARTING
9. BLOOD PRESSURE PULSE, SPO2 MONITORING
10. GRBS MONITORING 8TH HOURLY
11. INJ. METROGYL 500mg/IV/TID























Comments
Post a Comment