A 36 YEAR OLD MALE PATIENT WITH BREATHLESSNESS AnD DIFFICULTY IN SWALLOWING
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
Name : K. Supriya (9th semester)
Roll number : 53
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 36 YEAR OLD MALE PATIENT WITH BREATHLESSNESS AND DIFFICULTY IN SWALLOWING
Amc bed 1
A 36 year old male patient who is a watchman in a govt. Hospital came to the casuality with
C/C of BREATHLESSNESS and
DIFFICULTY IN SWALLOWING (even with Saliva ) Since 1 day .
Hopi:
This patient ,who is watchman by occupation since 20years ,wakes up at 5am in the morning ,goes for a walk and have his break fast at 8:30 am (rice &curry ),then he goes for COVID DUTIES (like reffering tests ) as his part time job since 2years ,before that he used to stay at home and have his lunch at 1:00pm (rice & curry),and have tea at 5:30 pm and goes to work as watchman ,and have dinner at around 8:30 pm and sleeps at 10:00pm (takes sound sleep of 8hrs). He has good relationship with his family ,friends .
He married 16years ago and have 2 girl child.
Patient was apparently asymptomatic before 2007 and then he developed breathlessness and difficulty in swallowing (even with Saliva ) he also noticed swelling of uvula ,for which he went to hospital in miryalguda.
They reffered him to hospital 2 (our management) where tracheostomy was done .
Past history:
Not a k/c/o DM/HTN/TB/BA.
No history of any other surgeries
Family history:
No similar family history
O/e:
Patient is conscious ,coherent and cooperative .
No signs of pallor or cyanosis or clubbing or icterus or koilonychia or lymphadenopathy.
Edema of limbs absent .
Edema of larynx present .
Edema of uvula present.
Vitals :
Temperature: Afebrile
Pulse Rate: 115 beats per minute
Blood pressure: 120 / 80 mm Hg
Respiratory Rate: 22 cycles per minute
SpO2: 98 % on room air
Systemic Examination:
1) RESPIRATORY SYSTEM :
* Chest is symmetrical and there are no chest deformities
* No wheeze, no crepts
* Bilateral air entry is present
* Normal vesicular breath sounds are heard
* Equal movements on both sides on respiration
2)CVS:
* S1 and S2 heart sounds are heard
* No murmurs
3) ABDOMINAL EXAMINATION:
* All quadrants of abdomen are moving equally with respiration
* Abdomen is soft & non-tender
* Bowel sounds are normal
4) CNS:
* No focal neurological deficits
* Higher motor functions are normal
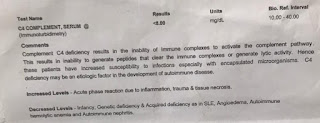
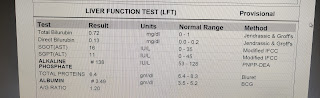
Investigations :
Diagnosis:
HEREDIATARY ANGIO EDEMA
Treatment:
1. INJ. HYDROCORTIONE 100 MG IV BD
2. NEB with ADRENALINE QID
Planning for FRESH FROZEN PLASMA Administration .
Day -1:
Treatment advice by ent department:
1. INJ. HYDROCORTIONE 100 MG IV QID
2. NEB with BUDECORT and ADRENALINE
3. Head end elevation

















Comments
Post a Comment